Blank Tb Test Form
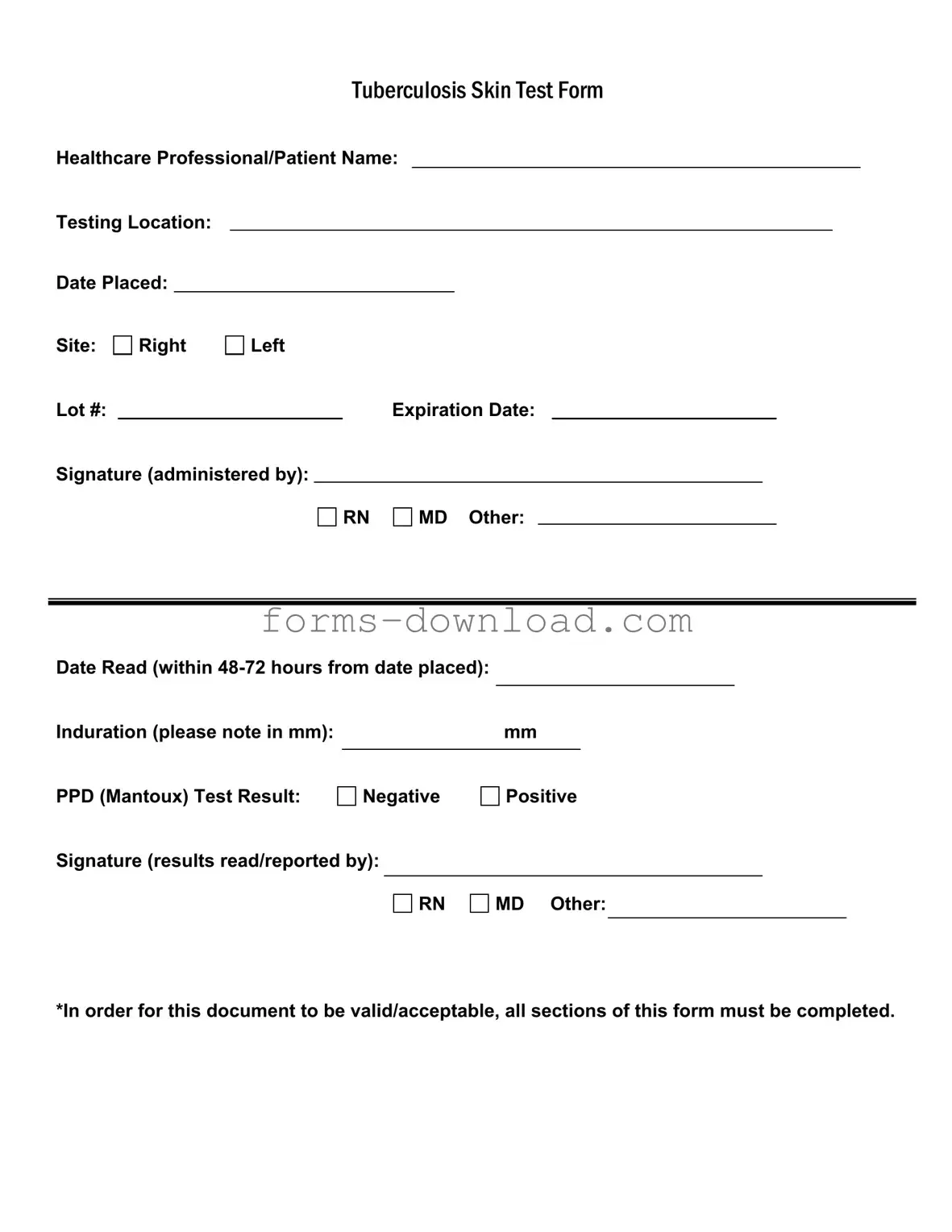
The Tuberculosis (TB) Skin Test Form is a critical document utilized in the assessment of individuals for tuberculosis exposure. This form captures essential information, including the names of the healthcare professional and patient, as well as the testing location. It records the date the test was placed and the specific site of administration, whether on the right or left arm. Each test is assigned a unique lot number and has an expiration date, ensuring that the test's validity is maintained. The signature of the administering healthcare professional, which may include a registered nurse (RN) or medical doctor (MD), is also required. The form stipulates that results must be read within 48 to 72 hours after placement, documenting the induration measurement in millimeters. The outcome of the PPD (Mantoux) test is clearly indicated as either negative or positive, with a signature from the professional who read and reported the results. It is imperative that all sections of this form are completed for it to be considered valid and acceptable.
More PDF Forms
Cash Drawer Balance Sheet - The form assists in maintaining transparency in financial operations.
For those unfamiliar with the process, the simple Motor Vehicle Bill of Sale form guide provides all the necessary steps to ensure your transaction is legally sound and efficient. This form is designed to facilitate a hassle-free vehicle sale and ensure that both parties have the documentation needed for a successful transfer.
Filing a 1099 Nec - The IRS provides guidelines on how to fill out this form correctly.
Dos and Don'ts
When filling out the TB Test form, it's important to follow certain guidelines to ensure accuracy and compliance. Here’s a helpful list of dos and don’ts:
- Do ensure all sections of the form are completed.
- Do double-check the testing location and dates.
- Do accurately note the induration measurement in mm.
- Do obtain the necessary signatures for administration and results.
- Don't leave any fields blank, as this could invalidate the form.
- Don't use incorrect abbreviations or terms that may cause confusion.
- Don't forget to record the expiration date of the lot number.
- Don't neglect to read the results within the specified time frame.
Tb Test Sample
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Listed Questions and Answers
-
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of a tuberculosis skin test, commonly known as the PPD (Purified Protein Derivative) test. This test helps determine if an individual has been exposed to the bacteria that cause tuberculosis. It is important for healthcare providers to keep accurate records of the test to ensure proper follow-up and treatment if necessary.
-
Who needs to fill out the TB Test form?
The form must be completed by both the healthcare professional administering the test and the patient receiving it. The healthcare provider will fill out sections related to the testing location, date placed, and their signature. The patient’s name and relevant details are also required to ensure that the test results are accurately linked to the correct individual.
-
What information is required on the TB Test form?
Essential information includes:
- Healthcare Professional/Patient Name
- Testing Location
- Date Placed
- Site of injection (Right or Left arm)
- Lot number and expiration date of the PPD
- Signature of the administering professional (RN, MD, etc.)
- Date Read (which should be within 48-72 hours from the date placed)
- Induration measurement (in mm)
- PPD Test Result (Negative or Positive)
- Signature of the professional reading/reported the results
-
How is the TB Test result interpreted?
The result of the TB Test is interpreted based on the size of the induration (swelling) at the injection site. A positive result typically indicates that the person has been exposed to the TB bacteria, while a negative result suggests no exposure. However, the interpretation can vary based on individual risk factors, so it’s essential to consult with a healthcare provider for a comprehensive evaluation.
-
What should I do if my TB Test result is positive?
If your TB Test result is positive, it is crucial to follow up with your healthcare provider for further evaluation. This may include additional tests, such as a chest X-ray or a sputum test, to determine if you have active tuberculosis. Early diagnosis and treatment are vital to prevent the spread of the disease.
-
Why is it important to complete all sections of the TB Test form?
Completing all sections of the TB Test form is essential for the document to be valid and acceptable. Incomplete forms may lead to confusion or miscommunication regarding test results and follow-up actions. Proper documentation ensures that all necessary information is available for healthcare providers to make informed decisions regarding patient care.
-
How long after the test is it read?
The TB Test must be read within 48 to 72 hours after it is placed. This timeframe is critical because it allows for accurate measurement of the induration. If the test is not read within this period, it may need to be repeated to ensure reliable results.
Form Overview
| Fact Name | Description |
|---|---|
| Form Title | The form is officially titled "Tuberculosis Skin Test Form." |
| Healthcare Professional/Patient Name | This section requires the name of the healthcare professional administering the test or the patient receiving it. |
| Testing Location | The location where the test is administered must be specified on the form. |
| Date Placed | The date when the test is administered needs to be documented accurately. |
| Induration Measurement | Induration must be measured in millimeters and recorded on the form. |
| Test Result | The result of the PPD (Mantoux) test must be indicated as either negative or positive. |
| Signature Requirement | Signatures from the administering healthcare professional and the person reading the results are required. |
| Completion Requirement | All sections of the form must be completed for the document to be valid and acceptable. |
| Governing Laws | State-specific forms may be governed by public health laws, such as those in California Health and Safety Code Section 120325. |